The narratives of patients with recurrent urinary tract infections and their experiences of diagnostic urine specimen collection
Introduction
A urinary tract infection (UTI) is a common infection which invades parts or the entire urinary tract, which consists of the kidneys, urethra and bladder (1) and predominantly caused by uropathogenic Escherichia coli (UPEC) which accounts for a large proportion of diagnosed UTIs (2). Patients with recurrent UTIs are defined as those who have experienced two episodes of acute bacterial cystitis, along with associated symptoms within the last six months or three episodes within the last year (3). Prudent antibiotic treatment is the conventional management for this bladder condition (4) and novel urinalysis using digital imaging has become a contemporary method for urine testing (5). UTIs are becoming more complicated and advanced novel treatment interventions are sought (6). Females are more affected than males, with more than 60% of females being diagnosed with a UTI in their lifetime (7). Female patients exhibit lower urinary tract symptoms (LUTS) such as dysuria (painful urination), urinary frequency, urinary hesitancy (slow to start urinary stream) and urinary urgency (urgent need to urinate) (8). The diagnosis and management of a UTI starts with patients providing a urine specimen for testing and microbial culture (9) however, the scrutiny of published text reveals that there is a gap in the literature that explores patient experiences of the management of recurrent UTIs through urine specimen collection and diagnostic testing.
Patients with a recurrent UTI who attend outpatient consultations are often requested to provide a urine specimen obtained by midstream specimen of urine (MSU) (10), catheter specimen of urine (CSU) (11) and also by using a novel urine collection device known as the Peezy MSUTM (12). Perspectives on urine specimen collection has evolved, with the idea that an invasive urine specimen collection method using a catheter provides an optimal specimen, but recent data has reported otherwise (13). The enthusiasm or willingness to provide a urine specimen for testing has not been evaluated and patient experiences have not been explored. Recent reports have highlighted the increasing use of urine collection devices for detecting the presence of an uncontaminated UTI (14) and women’s understanding of urine collection and sample contamination have been investigated (15). However, patient experiences and perceptions of using these urine collection devices have not been explored.
Patient experiences on providing a urine specimen has been a central focus point when it comes to sexual health management and screening procedures, and there is evidence that patients are accommodating of urine specimen testing for diagnosing a sexually transmitted infection (STI) in comparison to invasive vaginal swabs (16). This exploration has not been conducted for patients with recurrent UTIs, and it is fundamental in clinical practice that patient views, experiences and narratives are evaluated and embedded within clinical policies, guidelines and healthcare service provision (17). The objective of this study was to explore the narratives of patients with recurrent UTIs and their experiences of providing urine specimens for diagnosing and detecting the presence of an infection in the urinary tract.
This study explored patient experiences of a common clinical procedure of which is performed frequently for the detection of a UTI. Patients with a recurrent UTI repeatedly provide urine specimens for testing, but there remains a gap in the literature on patient experiences when providing a urine specimen for recurrent UTIs, and this area of enquiry is fundamental. We present this study in accordance with the SRQR reporting checklist (18) (available at https://aoi.amegroups.com/article/view/10.21037/aoi-22-3/rc), as this study adopted a qualitative approach which focused on individual experiences, patient narratives and which occurred in a clinical setting.
Methods
Study design
We conducted a descriptive-interpretive qualitative research study which Bradshaw et al. (19) deems the most appropriate method for this investigation, as it recognizes the subjective nature of the problem being explored, the different participant experiences and presents the findings in a way that reflects or closely resembles the research questions.
Study setting and population
The LUTS Service at Whittington Health is a specialist center providing scientific expert knowledge and care to patients diagnosed with LUTS and UTIs in London, United Kingdom. Patients diagnosed with complicated recurrent LUTS, were referred to the center by their family physician or urogynecologist for specialized treatment. The patients enrolled into this study were female, suffered from recurrent LUTS, were being treated for recurrent UTI and exhibited symptoms such as urinary hesitancy, overactive bladder (OAB), painful bladder syndrome (PBS), urinary incontinence and reduced quality of life as a result of their symptoms. The female patients were frequently reviewed at the outpatient center by health professionals working as part of a multiprofessional team which included a professor of medicine, consultant urogynecologist, junior doctors, nurses and microbiologists. All patients attending the center were familiar with center protocol and accustomed to providing a urine specimen for testing prior to consultation by either MSU, CSU, Peezy MSUTM device or naturally voided specimen without technique on varied consultation visits.
Convenience sampling was used for participant recruitment (19), as participants were drawn from the female patient population group attending the center for treatment of a recurrent UTI. The inclusion criteria were female patients over 18 years of age, diagnosed with a recurrent UTI and receiving treatment at the center for urinary hesitancy, OAB, PBS, urinary incontinence or general LUTS. The patients also had experience of providing a CSU, MSU, midstream urine using a Peezy MSUTM device, as well as providing a urine specimen that was naturally voided with no specified technique. The exclusion criteria were children, male patients, and female patients unable to provide informed consent.
All interested participants were given written information about study and were offered the opportunity to ask questions and address any concerns about participating. The participants who expressed willingness to take part in the study and who met the inclusion criteria received a formal invitation to participate in the study. Written informed consent and verbal consent were obtained directly from participants prior to study enrollment, and they were allocated a four-digit non-identifiable participant number for anonymity. Thirty female participants were recruited and granted permission to withdraw from the study at any time.
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013) (20). According to the National Research Ethics Service Committee (NRES) London-Harrow, the project was granted ethical approval (Ref-11/LO/1096).
Data collection and data analysis
Semi-structured interviews were conducted by an experienced and proficient doctoral research nurse, a member of the LUTS Service center, with the objective to explore the narratives of patients with recurrent UTIs and their experiences of providing urine specimens for diagnosing and detecting the presence of an infection in the urinary tract. The interview process was conducted over a period of eight weeks and took place in a quiet confidential meeting room within the center, which helped participants recollect thoughts and experiences of providing a urine specimen. Semi-structured interviews enabled the opportunity for probing, additional conversation and patient reflections on their experiences of providing a urine specimen for their recurrent UTI. Patient concerns that arose as a result of probing were addressed accordingly as part of follow-up consultations with senior clinicians. All interviews were recorded and lasted between 30 and 45 minutes for each participant. The semi-structured interviews consisted of four open-ended questions all of which were supported with question justifications (Table 1). The four questions were tested with colleagues at the LUTS Service prior to conducting the interviews to ensure the questions were clear, concise and accurate and to also evaluate the appropriateness of the interviewing skills. The semi-structured interviews were conducted face to face and data were audio recorded and transcribed verbatim.
Table 1
| Question number | Question asked | Justification |
|---|---|---|
| Interview question 1 | Which method of urine collection did you prefer and why? | Patients are most likely to think of urine specimen collection methods they were comfortable with in comparison to what was least preferred |
| Interview question 2 | Which method of urine collection did you not like and why? | It was important to establish what patients were not enthusiastic about when it was related to providing a urine specimen for diagnosing their recurrent urinary tract infection |
| Interview question 3 | What method of urine collection do you think provided the cleanest sample and why? | Patient thoughts and perceptions frame the way they engage with management of their recurrent bladder infection. It was essential to obtain their perspectives on what they regarded as a clean urine specimen |
| Interview question 4 | Which method of urine collection do you think should be used as a standard method and why? | Attending the Lower Urinary Tract Symptoms Service at Whittington Health was a regular occurrence for treatment and management of their recurrent urinary tract infection. Obtaining perspectives on what should be a standard method for urine specimen collection was fundamental |
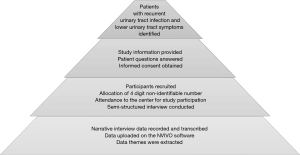
The interview questions were designed to understand and interpret the lived experiences (21) from patients diagnosed with recurrent UTIs and the events that occur whilst providing a urine specimen for diagnosing the presence of an infection. The four interview questions were asked in order to obtain patient narratives of providing urine specimens for diagnostic testing by four different specimen collection methods, of which they had performed (Appendix 1). All recorded interview data were transcribed verbatim in preparation for the analysis (22). The transcribed data were uploaded to the NVIVO software to organize and group together the transcribed data into identified themes (23). Both researchers experienced with the NVIVO software reviewed transcribed data to ensure trustworthiness and rigour throughout the data analysis process. The interview process was discontinued when there was evidence of no new data emerging and responses became repetitive. Figure 1 summarizes the recruitment process that led to data collection.
Results
Theme 1: uncomplicated urine specimen collection
Thirty semi-structured interviews were conducted, and four themes had emerged from the narrative data (Table 2). Each participant expressed the need and ability to provide a urine specimen that was comfortable and effortless when diagnosing an acute flare of bladder symptoms and UTI. Providing a urine specimen naturally and without any method or technique was repeatedly regarded as uncomplicated, straightforward and the ideal procedure for obtaining a urine specimen for diagnostic testing.
Table 2
| Data themes |
| Theme 1: uncomplicated urine specimen collection |
| Theme 2: painful catheter urine specimen |
| Theme 3: the superior catheter urine specimen |
| Theme 4: naturally voided urine as standard clinical practice |
“I prefer the pee in the pot. It is easier because when I need to give a sample I’m always desperate to go, and doing the wiping and collecting the middle part of the stream on the midstream sample delays the urine process and the urine starts to come out before I’m ready to collect it” (Participant 3456).
“The straightforward pee in the pot. Because it’s simple and easy, you don’t have to prepare for it. Ease of use. I would go for just straightforward peeing as any doctor’s office would not have the time to do it any other way. I find that a majority of toilets are not designed for collecting midstream urine. It’s difficult to get a midstream because it’s hard to judge when you actually get the midstream, and you sometimes end up urinating on your hands” (Participant 3963).
The participants often expressed that, patients like them with a history of recurrent UTIs should be able to provide a urine specimen that was rapid, effortless and requiring no technique due to their complex bladder symptoms. The MSU and the Peezy MSUTM were regarded as complicated in comparison to the natural way of voiding urine. The varied views and perspectives towards the MSU and the Peezy MSUTM specimen collection methods were evaluations of concern, challenging thoughts and lack of understanding on how correctly perform the task. Although providing a urine specimen by these methods was not an uncommon request, collecting the middle part of a urinary stream remained an awkward idea.
“The MSU can be tricky and a bit messy and it has caught me out a couple of times. It depends on the circumstances, but the easiest thing is for people to urinate in the pot” (Participant 2977).
“I still think the midstream is the awkward one. I don’t know when to gauge the midstream part of the urine. I’m always confused with this one. The toilet height is awkward as well for collecting the midstream. It’s easier to get an infection doing all these steps. I hate that sample because it is so awkward to collect” (Participant 3178). “The midstream was difficult using the utensils to get a midstream sample” (Participant 2576).
“I wasn’t keen on the ‘Peezy’ as I needed an extra pair of hands, and I didn’t trust the instruction provided in the pack” (Participant 3600). “I didn’t like the Peezy because I couldn’t work out how it worked and I was worried it was going to disconnect and I would end up peeing all over the floor” (Participant 4014).
“The Peezy, it was confusing; I needed a demonstration of how to use the device. I wasn’t sure whether I was to stand up or sit down when using the device” (Participant 4265).
Theme 2: painful catheter urine specimen
Most of the participants attending the LUTS Service had a history painful bladder symptoms at some point during consultations and follow-up reviews. Pain was greatly experienced with the catheter specimen method, as some of the participants were being treated for pain symptoms as a result of recurrent UTIs. The experience of catheter insertion into the bladder to obtain a urine specimen heightened the narrative of pain.
“The catheter gives you a horrible sensation after, as if you want to go, but there is nothing there. I feel as though it will enhance an infection as I have experienced this in the past and because it is a foreign body” (Participant 2365).
“I did not like the catheter, because of the discomfort, and I have had a bad reaction to it in the past” (Participant 3965). “I don’t like the catheter. Because it feels invasive, I have had it done before and I bled afterwards. I also felt sore for a couple of hours afterwards” (Participant 3456).
Theme 3: the superior catheter urine specimen
The catheter urine was regarded as the optimal urine specimen by the participants, and pain was endured for the purpose of obtaining the purest urine specimen.
When the participants shared their thoughts on the urine specimen collection method perceived to be optimal, there were positive responses in favour of the catheter specimen of urine. There was a strong ethos that the catheter urine specimen was superior and ideal for patients blighted with a recurrent UTI.
“I feel the catheter provided the cleanest sample, because it goes straight up and does not touch any other part of the area” (Participant 2365).
“I think the catheter, as I would have thought you get a more accurate reading if there was any infection” (Participant 2131). “I would assume the catheter, because it is direct into the bladder and there is nothing else intervening” (Participant 2386). “Well I always thought the catheter because to me it seems the purest way and least method of contamination” (Participant 2576).
“The catheter provided the cleanest sample as it is all internal and it’s the cleanest way of collecting the sample” (Participant 4014). “I guess the catheter would be asked for if we wanted to eliminate contamination” (Participant 2587).
Theme 4: naturally voided urine as standard clinical practice
When exploring the narratives of patients with recurrent UTIs and their experiences of providing urine specimens for diagnostic testing, it was evident that naturally voided urine should be recognized as a standard urine specimen collection method in clinical practice. The participants were of the notion that a naturally voided urine specimen would be ideal for patients without a diagnosis of complicated recurrent UTIs. And patients with a complicated bladder would require specialist diagnosis, extensive investigations and specialized treatment interventions.
“I think that urinating everything into a pot is more reliable as you can detect whatever bacteria are there. It will give a true record of infection” (Participant 2365). “I think the standard practice should be the method that provides the cleanest sample. But from the patients perceptive the pee in the pot should be standard” (Participant 3456). “I guess the pee in the pot should be standard practice, as you have more control over it and more privacy as well. You can do it yourself, nobody else is needed” (Participant 4369). “I think pee in the pot, because I suppose the pee in the pot will give the same results as an MSU. It’s natural and you don’t have to think about doing anything. The midstream is difficult as you don’t know when your catching the midstream” (Participant 2287).
Discussion
Four themes emerged when exploring the narratives of patients with a recurrent UTI and their experiences of providing a urine specimen for diagnosing the presence of an infection. The interview data highlighted the importance of being able to provide a urine specimen naturally, without any method or technique and in a straightforward manner for someone diagnosed with a recurrent UTI. Rapid and effortless urine specimen collection was the main focus from the narratives expressed by the participants. Rapid screening of urine specimens in current practice is fundamental, it hastens the results of urine cultures and is the deciding factor for antibiotic treatment for hospitalized older adults with UTIs (24).
Although pain symptoms were experienced with the catheter specimen method, the participants collectively believed that the catheter was the optimal method for obtaining a urine specimen. The narrative data also suggests that the catheter specimen reduced the chances of urinary contamination and was regarded the best method for patients diagnosed with a recurrent UTI. The compelling notion that the catheter specimen of urine would provide the true identification of a UTI was considered the gold standard from the participants perspective and was regarded as the optimal method. Recent data published as part of this investigation has revealed that this was not the case, and that the catheter specimen actually bypassed the cells and sediments that were at the base of the bladder, which were crucial for diagnosing the presence of an infection (13). The findings from our earlier study also revealed that the spun sediment culture performed on non-invasive samples was the most productive method for identifying bladder pathology and the urine specimens obtained with a catheter had significantly more negative results (13).
The participants were fixated on the concept of having a urine specimen that was uncontaminated and that would identify the true pathology of their recurrent UTI. The MSU, Peezy MSU™ and naturally voided urine specimens were not considered appropriate methods for a population diagnosed with a recurrent UTI, who in their opinion required an accurate diagnosis of their infection.
The narrative that focused on naturally voided urine as standard clinical practice, was collective and primarily centered towards patients with an uncomplicated bladder when providing a urine specimen for diagnostic testing. The participants notion was that, naturally voided urine specimens would be favorable for patients without diagnosis of a complicated recurrent infection or LUTS. Their narratives justified the need for more invasive scrutiny of urine specimens for patients with a complicated bladder that requires specialist diagnosis, extensive investigations and specialized treatment interventions.
Clinical implications
The patients attending the LUTS Service at Whittington Health, are prescribed a comprehensive treatment plan that evaluates symptoms, urine specimens, medication tolerance, and now fundamentally, the inclusion of their narratives to consolidate the holistic approach for diagnosing and detecting the presence of their UTIs. Encouraging the practice of urine specimen collection that reveals the true pathology of the bladder should be considered and incorporated in clinical practice for patients with a recurrent UTI. Further research on patient experiences when diagnosing and detecting the presence of a UTI is fundamental and narratives should be considered in the management of recurrent illnesses.
Methodological considerations
To ensure the credibility of this study, it is essential that we address a key element which is rigor of the sampling method (22). Although we used convenience sampling from the patient population group attending the LUTS Service at Whittington Health, this sampling method poses a potential lack of representation of a population with recurrent UTIs as a whole. Recruiting from a diverse patient population group attending a clinical treatment center like the LUTS Service may overcome this challenge.
Conclusions
Exploring the lived experiences of patients through the journey of urine specimen collection, diagnostic urine testing and management of their recurrent UTI is fundamental. The importance of patient experiences is that it highlights patient challenges, concerns, their own personal beliefs, and influences changes in clinical practice (25). The interview data revealed the varied perceptions of urine specimen collection and highlights the challenges patients encounter during the diagnostic stages of a recurrent UTI.
Acknowledgments
We the authors dedicate this manuscript in honor of Late Professor James Malone-Lee (University College London, United Kingdom). Professor James Malone-Lee was our mentor, our doctoral supervisor, and the founder of the Lower Urinary Tract Symptoms (LUTS) Service at Whittington Health, London, United Kingdom.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the SRQR reporting checklist. Available at https://aoi.amegroups.com/article/view/10.21037/aoi-22-3/rc
Data Sharing Statement: Available at https://aoi.amegroups.com/article/view/10.21037/aoi-22-3/dss
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at https://aoi.amegroups.com/article/view/10.21037/aoi-22-3/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). According to the National Research Ethics Service Committee (NRES) London-Harrow, the project was granted ethical approval (Ref-11/LO/1096). All participants were informed about the project verbally and in writing and were guaranteed anonymity with the allocation of a four-digit non-identifiable participant number. Written and oral consent was obtained from all participants prior to study enrollment and for publication of data.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Salari N, Karami MM, Bokaee S, et al. The prevalence of urinary tract infections in type 2 diabetic patients: a systematic review and meta-analysis. Eur J Med Res 2022;27:20. [Crossref] [PubMed]
- Klein RD, Hultgren SJ. Urinary tract infections: microbial pathogenesis, host-pathogen interactions and new treatment strategies. Nat Rev Microbiol 2020;18:211-26. [Crossref] [PubMed]
- Aydin A, Ahmed K, Zaman I, et al. Recurrent urinary tract infections in women. Int Urogynecol J 2015;26:795-804. [Crossref] [PubMed]
- Asma B, Vicky L, Stephanie D, et al. Standardised high dose versus low dose cranberry Proanthocyanidin extracts for the prevention of recurrent urinary tract infection in healthy women PACCANN: a double blind randomised controlled trial protocol. BMC Urol 2018;18:29. [Crossref] [PubMed]
- Szmulik M, Trześniewska-Ofiara Z, Mendrycka M, et al. A novel approach to screening and managing the urinary tract infections suspected sample in the general human population. Front Cell Infect Microbiol 2022;12:915288. [Crossref] [PubMed]
- Rando E, Giovannenze F, Murri R, et al. A review of recent advances in the treatment of adults with complicated urinary tract infection. Expert Rev Clin Pharmacol 2022;15:1053-66. [Crossref] [PubMed]
- Foxman B, Brown P. Epidemiology of urinary tract infections: transmission and risk factors, incidence, and costs. Infect Dis Clin North Am 2003;17:227-41. [Crossref] [PubMed]
- Bono MJ, Reygaert WC. Urinary Tract Infection. StatPearls. Treasure Island (FL): StatPearls Publishing StatPearls Publishing LLC.; 2018.
- NICE. Urinary tract infections in adults. In: England N, editor.: National Institute for Health and Care Excellence.; 2015.
- Dougherty L, Lister S, West-Oram A. The Royal Marsden Manual of Clinical Nursing Procedures (Royal Marsden Manual Series). 9th Edition ed. West Sussex: Wiley Blackwell; 2015.
- Iggulden H, MacDonald C, Staniland K. Clinical skills: the essence of caring. Berkshire: Open University Press; 2009.
- Collier S, Matjiu F, Jones G, et al. A prospective study comparing contamination rates between a novel mid-stream urine collection device (Peezy) and a standard method in renal patients. J Clin Pathol 2014;67:139-42. [Crossref] [PubMed]
- Collins L, Sathiananthamoorthy S, Rohn J, et al. A revalidation and critique of assumptions about urinary sample collection methods, specimen quality and contamination. Int Urogynecol J 2020;31:1255-62. [Crossref] [PubMed]
- Hayward G, Mort S, Yu LM, et al. Urine collection devices to reduce contamination in urine samples for diagnosis of uncomplicated UTI: a single-blind randomised controlled trial in primary care. Br J Gen Pract 2022;72:e225-33. [Crossref] [PubMed]
- Glogowska M, Croxson C, Hayward G. Women's information needs around urine testing for urinary tract infections: a qualitative study. Br J Gen Pract 2022;72:e244-51. [Crossref] [PubMed]
- Bilardi JE, De Guingand DL, Temple-Smith MJ, et al. Young pregnant women's views on the acceptability of screening for chlamydia as part of routine antenatal care. BMC Public Health 2010;10:505. [Crossref] [PubMed]
- Sheppard MK. Fallacy or Functionality: Law and Policy of Patient Treatment Choice in the NHS. Health Care Anal 2016;24:279-300. [Crossref] [PubMed]
- O'Brien BC, Harris IB, Beckman TJ, et al. Standards for reporting qualitative research: a synthesis of recommendations. Acad Med 2014;89:1245-51. [Crossref] [PubMed]
- Bradshaw C, Atkinson S, Doody O. Employing a Qualitative Description Approach in Health Care Research. Glob Qual Nurs Res 2017;4:2333393617742282. [Crossref] [PubMed]
- The World Medical Association. WMA Declaration of Helsinki – Ethical principles for medical research involving human subjects. Available online: https://www.wma.net/policies-post/wma-declaration-of-helsinki-ethical-principles-for-medical-research-involving-human-subjects/2016
- Reiners GM. Understanding the differences between Husserl’s (descriptive) and Heidegger’s (interpretive) phenomenological research. Journal of Nursing Care 2012;1-3.
- Burkholder GJ, Cox KA, Crawford LM, et al. Research Design and Methods. USA: SAGE Publications, Inc.; 2019.
- NVIVO. Fueling Academic Research With World-Class Data Analysis Software; 2022 Available Online: https://www.qsrinternational.com/nvivo-qualitative-data-analysis-software/about/nvivo/who-its-for/academia
- Choi JJ, McCarthy MW, Meltzer KK, et al. The Diagnostic Accuracy Of Procalcitonin for Urinary Tract Infection in Hospitalized Older Adults: a Prospective Study. J Gen Intern Med 2022;37:3663-9. [Crossref] [PubMed]
- Tebb KP, Paukku MH, Pai-Dhungat MR, et al. Home STI testing: the adolescent female's opinion. J Adolesc Health 2004;35:462-7. [Crossref] [PubMed]
Cite this article as: Collins L, Khasriya R. The narratives of patients with recurrent urinary tract infections and their experiences of diagnostic urine specimen collection. Ann Infect 2022;6:2.